Anal fissures are unfortunately a common cause of rectal pain and bleeding. This pain or bleeding can significantly limit a person’s ability to sit, to empty the bowels comfortably, or to participate in work and leisure activities. The good news is that properly trained pelvic rehabilitation clinicians are able to help you heal this painful condition and learn how to manage flare-ups when they happen.
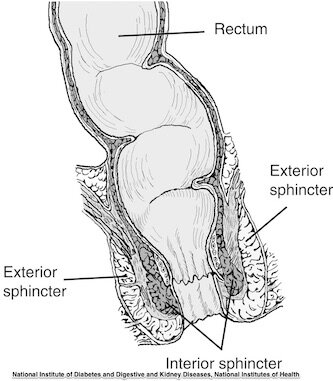
A rectal fissure, or tear in the lining of the anal canal, is sometimes described like a paper cut. This small yet sensitive tear can first happen when someone passes a large or hardened bowel movement, so constipation is in general associated with fissures. Surgery or injury to the canal can also create a fissure, and once the tear takes place, re-injury to that tissue can happen. One theory on why some folks get fissures and others do not is that some people have a really tight anal canal and tight pelvic floor muscles. The anal canal has an external and an internal sphincter, with the external made up of skeletal muscle (muscle that you can contract and relax by thinking about it) and the internal sphincter is made up of smooth muscle (muscle tissue that your central nervous system operates). If either of these sphincters become too tight, the tension, pressure, and lack of blood flow may contribute to a fissure formation or make it difficult for an existing fissure to heal.
What can you do to help avoid or heal a fissure? Staying hydrated and eating a diet that promotes softer stools can help. Visiting a gastrointestinal or colorectal specialist to keep an eye on your healing is important as well. Some providers will prescribe a medicine that helps the smooth muscle in the anal canal relax. Beyond that, many fissures heal on their own with time, perhaps warm baths, and through keeping the bowels healthy. What if the fissure becomes chronic, or causes severe pain and bleeding? Bleeding that is outside of normal may have to be managed by a surgical approach, but much of the time it is the pain and difficulty passing stool that is problematic.
How does pelvic rehab address the issue of fissures? Interestingly, providing gentle manual therapy to the anal canal and pelvic muscles can be a huge help in speeding recovery and in reducing flare-ups. This manual therapy can involve placing a gloved, examining finger in the anal canal and applying gentle pressure to help the soft tissues relax and become less tender. A person can also learn to be more aware of any tendency to hold these muscles tight (fairly natural to tension these muscles if there is pain), and to relax when holding is noticed. If there is a healing scar from a fissure, this soft tissue can also be very gently worked on to help desensitize the pain and to improve blood flow and scar mobility. It can seem counterintuitive that this painful tissue can improve with pressure applied to it, but we see this condition frequently in the clinic, and fortunately the body is able to heal this tear and with healing, the pain and bleeding resolve. Deep breathing, learning how to empty the bowels properly with coordination between the abdominal wall and pelvic floor muscles, and having healthy nutrition and activity levels can also play a part in recovery.
Regardless of how long a person has dealt with an anal fissure, pelvic rehabilitation can quickly make gains in discomfort and bleeding. Many providers have no idea that pelvic health can help heal fissures, and if you have any questions about your condition, feel free to reach out for answers. It’s important to work with a pelvic health provider that has specific training in colorectal health, and all providers at Flow have had this training. We work closely with medical providers to help a patient find the best pathway to recovery.