Vasectomy is a common contraceptive technique that interrupts the pathway through which the sperm travels. Most people recover well with simple techniques such as short-term rest and ice packs. Others develop severe pain in the region of the scrotum and spermatic cord that can limit work, sitting, movement, sleep, sexual health and other activities. Post-vasectomy pain can be treated successfully with pelvic rehabilitation, yet this fact remains widely unknown.
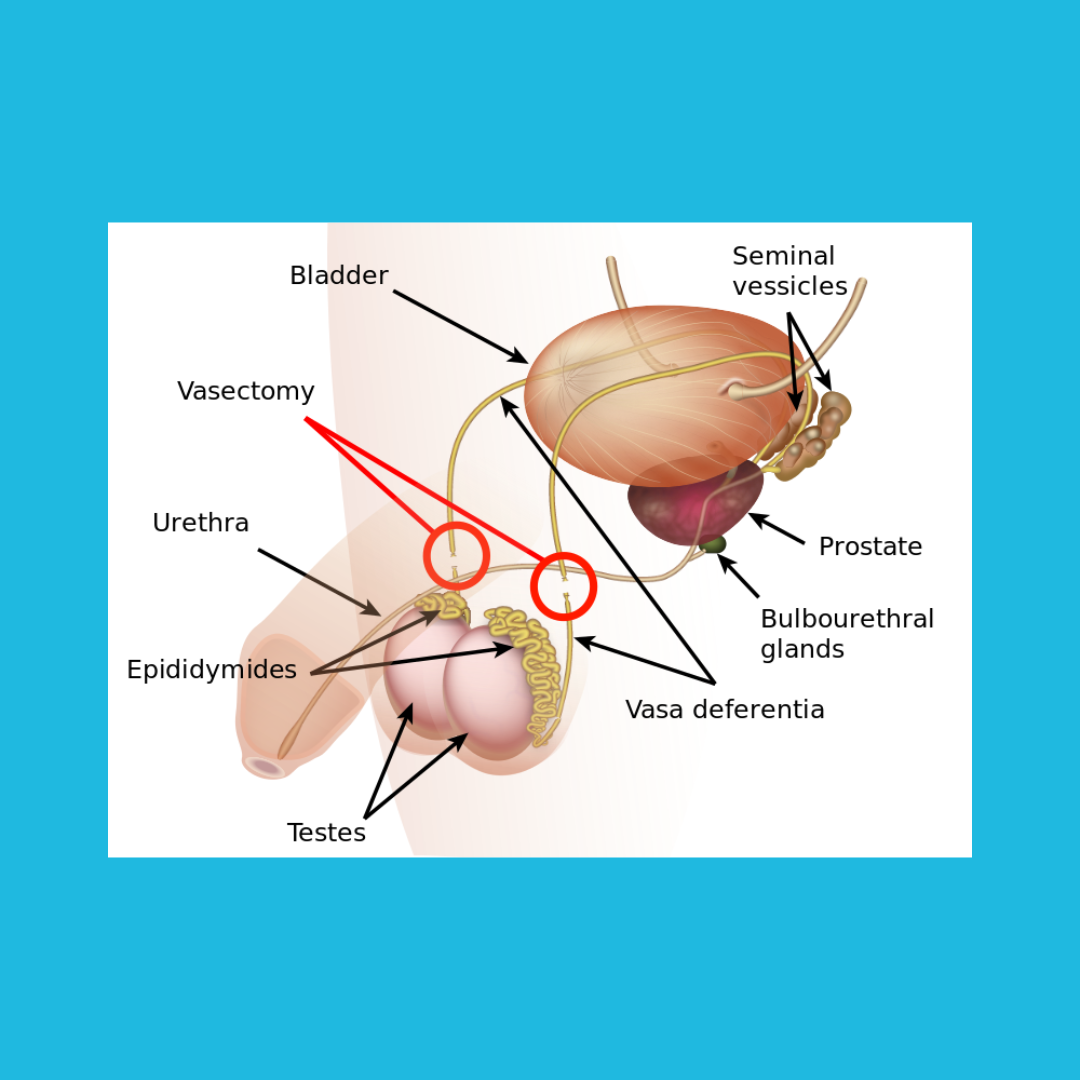
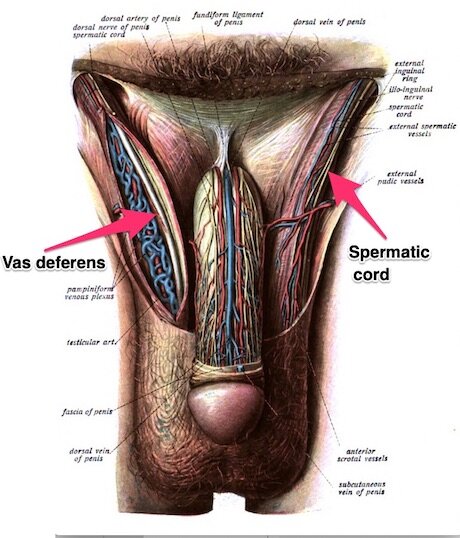
There are different techniques used to interrupt the vas deferens, and regardless of the approach used, new onset pain may occur. To understand the common area of dysfunction, it is helpful to be familiar with the anatomy. The spermatic cord travels from the lower abdomen to the scrotal area. Through this cord you will find the vas deferens, a tube that extends from the epididymis all the way into the abdomen and behind the bladder where it can deliver sperm to the urethra. The vas deferens is typically cut or disrupted at a location that can be easily reached in an outpatient procedure, accessed via the scrotal tissues.
The location where the cut or disruption is made can develop a sperm granuloma, which clinically may be palpable as a thick, hard nodule. Palpation to the area of the granuloma and nearby tissues can often reproduce the sharp, searing pain that is reported. Other symptoms may include a dull throbbing, nerve-like pain, or a hypersensitivity to touch or pressure on the tissues. In clinical experience, gentle palpation and mobilization of the painful area can not only decrease the size of the granuloma, but reduce the symptoms as well. This may only require a few visits and techniques instructed to continue with care at home. Because of the pain, nearby muscles may also become tense and sore. The sooner these concerns are addressed, the better. If you have questions about your recovery from vasectomy and and concerned about your symptoms, check in with a pelvic health therapist who can provide tools for healing.